by Dr Laila Kaikavoosi
What is Osteoporosis and what are the symptoms:
Osteoporosis literally means ‘porous bone’. It causes bones to become weak and fragile. It is not a painful condition and people with this condition generally do not have any symptoms. They may not even know they have osteoporosis unless they are either tested for it or their bones become so brittle that a fall or even a stress as mild as bending or coughing causes a fracture. In these circumstances pain can be intense and chronic.
Osteoporosis related fractures commonly occur in the spine, hips or wrists.
Our bones are constantly renewing themselves. New bone is made by cells called osteoblasts and old bone is broken down by cells called osteoclasts. Bone cells are connected together by strong bonds.
Factors which could increase the risk of developing Osteoporosis:
Ethnicity
Whites and Asians are at higher risk, although both men and women of all ethnicities can be affected.
Sex
Women are at higher risk of developing osteoporosis, especially after menopause when their hormone levels drop.
Body frame
The lower the BMI (body mass index) and smaller frame tend to have a higher risk of developing osteoporosis. This can be due to the genetic makeup of a person or secondary to an eating disorder.
Family history
Having a parent or sibling with osteoporosis put us at higher risk, especially if our mother or father suffered a fractured hip.
Age
The older we get the balance between bone formation and break down can be disturbed due to a number of reasons including the process of ageing itself as well as a result of a chronic disease or medications.
Lifestyle
Smoking, excessive alcohol consumption, inactivity and unhealthy diet puts us at increased risk of developing osteoporosis.
Medical conditions and medications
Some medical conditions like celiac disease, IBD (inflammatory bowel disease), cancer, Rheumatoid arthritis plus treatments which are used to treat conditions like cancer, gastric reflux, seizures and transplant rejection can also contribute to development of osteoporosis.
Hormone function
We know that Progesterone helps make new bone and oestrogen helps reduce the break-down of bone. Additionally, testosterone makes the bonds between bone cells stronger. This is why a woman who has considerably less hormones after her menopause is at a higher risk of developing osteoporosis
Men also have an increased risk of developing osteoporosis as they age but the reduction in their testosterone levels are more gradual and therefore their risk is less frequent.
Thyroid levels are also important players in our bone health and strength. Too much thyroid hormone can result in osteoporosis.
How to prevent and treat osteoporosis
Hormone replacement therapy (HRT): replacing estrogen, progesterone and testosterone in peri-menopausal and menopausal women can prevent and /or reduce their risks of developing osteoporosis. Currently, there is no data to suggest what level of blood hormonal level we should aim for, but we know that replacing hormones in women who either have a strong family history of osteoporosis or are at higher risk of developing this condition protects against it.
Lifestyle modifications
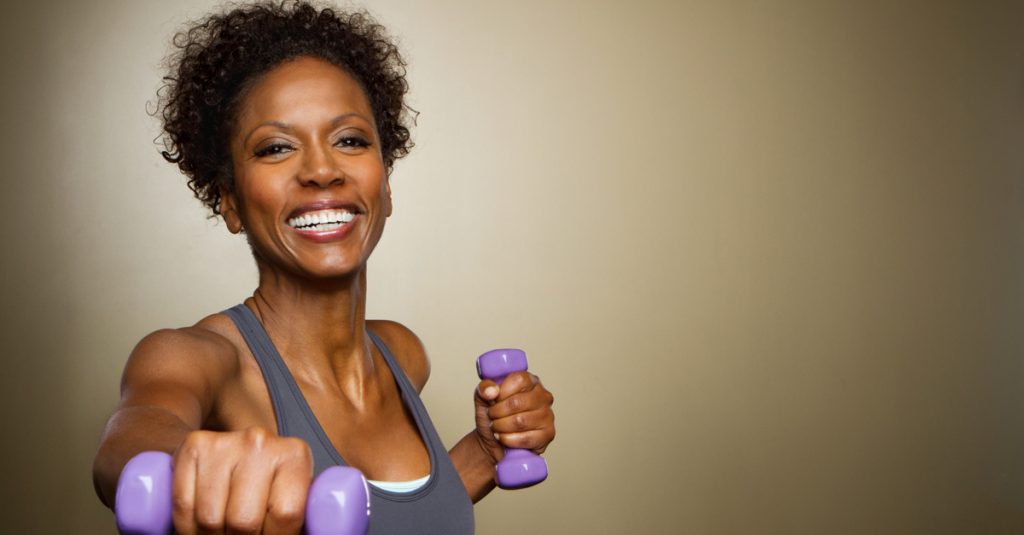
Exercise
Weight bearing exercises. Any weight bearing exercise that promotes good posture and balance is helpful for your bones specially running, jumping, walking, weightlifting and dancing.
Nutrition
An important part of preventing and managing osteoporosis is good nutrition.
Calcium
Calcium is one of the building blocks of bone and critical to bone health. Low calcium levels contribute to reduced bone density and increased bone loss. The recommended daily intake for most adults is 1000-1200 mg per day. Food that are high in calcium are dairy products but also kale, broccoli and calcium-fortified cereals and tofu products.
Vitamin D is essential in absorption of calcium and therefore calcium supplements should not be taken alone. Magnesium helps direct the calcium to the bone, keeping it out of soft tissue.
There are still some controversies around the correct amount of calcium intake as some experts suggest that excessive intake of calcium can result in heart disease and it has certainly been linked to development of kidney stones.
Sources of Protein and Fat
Protein is an important part of bone tissue and so it plays a major role in bone health. Plant proteins such as nuts and beans as well as fish and lean meat like skinless chicken are the best choices. Plant proteins are rich in vitamins, minerals and estrogen-like compounds that help maintain bone health.
Dairy like low fat milk and plain yogurt are also beneficial.
Protein should account for 25-35% of you total daily calories.
Good fat is also crucial for your body to function properly. Monounsaturated fats such as olive oil, nuts and seeds, avocado, cold water fish provide the essential omega-3 fatty acids (eicisapentaenoic acid (EPS) and docosahexaenoic acid (DHA). But we must remember to eat these, like everything else in moderation as too much can be harmful. Avoid saturated fats as these can be detrimental to bone health.
Fruits and Vegetables
These are generally low in calorie and fat and high in fibre and essential vitamins and minerals. Our aim should be to have 4+ servings of vegetable and 3 servings of fruit each day.
Fruits and vegetables are great sources of vitamins A,C,K plus potassium and magnesium. All of which play an important role in bone health.
Whole grains equally contain high levels of fibre and magnesium and should be included in our daily diet.
Smoking
Giving up smoking and reducing alcohol intake all have been shown to have a positive effect on bone mineralisation and health.
Reduce alcohol and caffeine consumption
Consuming 1-2 alcoholic drinks a day increases the rate of bone loss and reduces our ability to absorb calcium. Drinking alcohol with meals reduces the calcium absorption.
Caffeine can increase the rate of calcium loss in urine. Moderate caffeine intake, roughly 2-3 cups of coffee per day, won’t be harmful specially if your diet contains adequate calcium.
Reduce sugar, salt and phosphate additives
Too much salt intake can result in increased excretion of calcium in urine. Our daily consumption of salt should be limited to 2300mg daily. This is equivalent to one teaspoon!
Phosphorus is a common additive in processed food. This can reduce calcium absorption from our small intestine. Always try to choose fresh food instead of processed ones.
Exercise
Weight bearing exercises have been shown to be very effective at maintaining bone density. These can be high intensity like running, dancing, jumping or low intensity like walking or climbing stairs
Muscle strengthening exercises are also very important to improve and maintain bone strength. Exercises which improve posture and balance like yoga and pilates are helpful in prevention of falls.