Menopausal joint pain is characterised by joint soreness and is caused mostly by a decline in oestrogen levels, which frequently leads to an increased risk of musculoskeletal injury and faster bone and muscle loss.
Oestrogen levels dropping during menopause has been related to a higher risk of osteoarthritis (OA) and stiffness in the joints developing or getting worse. Joint pains impact 50% or more of menopausal women and can be effectively managed with a combination of lifestyle changes, medication, and alternative therapy.
What is Menopausal Joint Pain?
Menopausal joint pain, also known as menopausal arthralgia, is a symptom of menopause that is characterised by pain, stiffness, or discomfort in the joints. The shifting hormone levels, particularly the decline in oestrogen, has a substantial impact on joint health as women approach menopause. These pains are frequently observed in joints such as the neck, shoulders, elbows, and knees.
Menopausal status, BMI, work status, and depressed mood were all connected with the feeling of troublesome aches and stiff joints, according to a study undertaken by Szoeke et al from the Department of Psychiatry, University of Melbourne. Aches and stiff joints are frequent in postmenopausal women, but they do not always indicate radiological osteoarthritis.
While menopausal joint pain is a well-known complaint, understanding its underlying causes, which include but are not limited to hormonal changes, is essential. Speak with us at OMC so our highly-experienced female doctors and nurses can further review your condition and give you professional advice.
In the following sections we’ll further explore the factors that contribute to joint pain and explore some research to better help you understand the ins and outs of this symptom.
What Causes Joint Pains During Menopause?
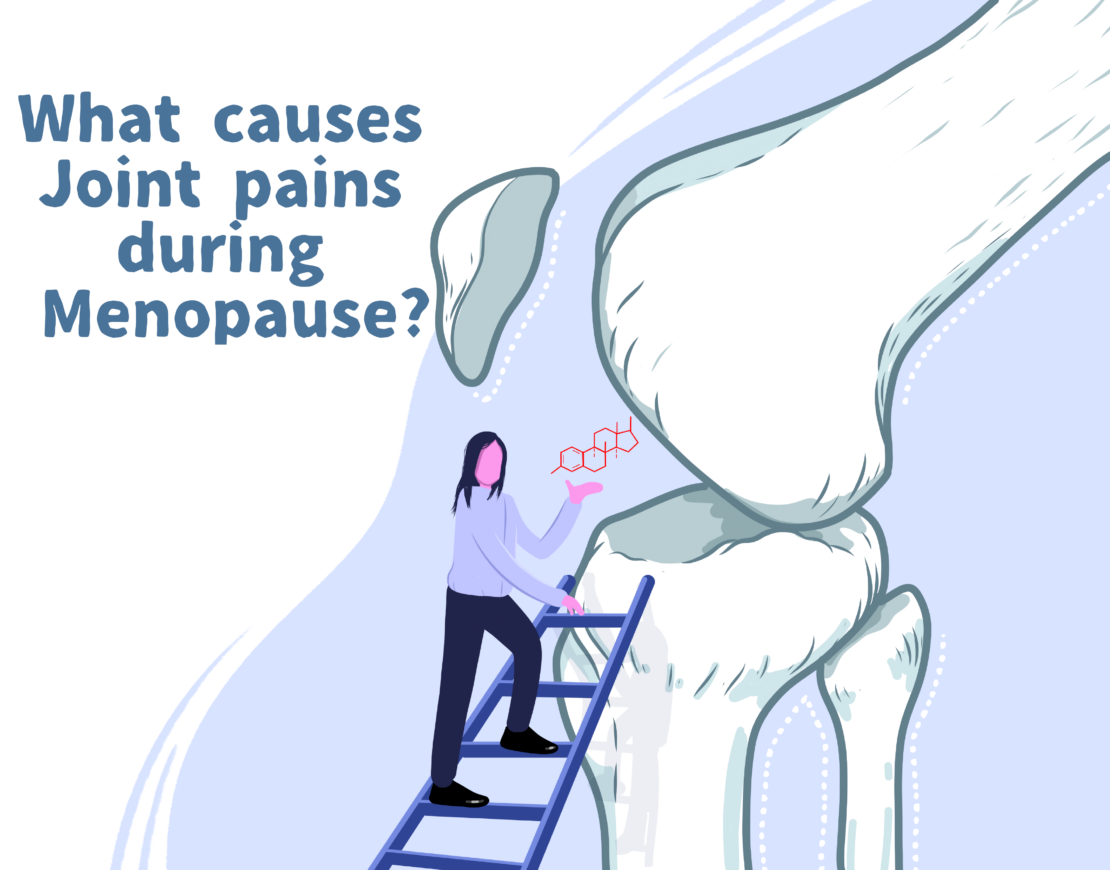
The eventual drop in oestrogen levels is the primary cause of joint aches during menopause. Oestrogen has anti-inflammatory qualities, and as levels of this hormone drop after menopause, it can lead to increased inflammation and joint discomfort. It also reduces stiffness in tendons and ligaments, which has a direct impact on performance and injury rates.
According to a study conducted by the Biomedical Engineering Graduate Group at the University of California, oestrogen receptors are found in all musculoskeletal tissues, including muscle, bone, ligament, and tendon. Oestrogen is known to affect metabolism inside various tissues. Menstruating women had more ACL ruptures than men, indicating that oestrogen has a role in regulating musculoskeletal function, and menopause is associated with an increased risk of musculoskeletal injury, faster bone and muscle wastage, and lower sensitivity to anabolic stimuli.
Addressing joint pain during menopause necessitates an understanding of the symptom’s prevalence. Expanding on this, the following section will investigate how many women have joint pain as part of their menopausal journey, emphasising the importance of awareness and focused therapies.
How many women normally suffer from menopause joint pains?
Research findings suggest that joint pains affect 50% or more of women during their menopausal transition. According to Malgorzata Magliano of Stoke Mandeville Hospital in Aylesbury, more than half of the women have menopausal joint problems or arthralgia around the time of menopause. The reasons for joint pain in postmenopausal women can be difficult to pinpoint because menopause coincides with an increase in the prevalence of chronic rheumatic disorders such as osteoarthritis.
Nonetheless, the prevalence of arthralgia appears to rise in menopausal women, which is assumed to be due to a decrease in oestrogen levels. A similar phenomenon happens after abrupt discontinuation of hormone replacement therapy or treatment with aromatase inhibitors.
This symptom’s prevalence and damaging nature highlight the need for better treatment techniques. As we gain a better understanding of joint pain in the context of hormonal fluctuations, the next logical issue is whether hormone replacement therapy (HRT) can provide relief, which we shall discuss in the following section.
Can HRT alleviate the symptoms of Joint Pains During Menopause?
Yes, Hormone Replacement Therapy (HRT) can alleviate joint pains associated with menopause. Hormone replacement treatment (HRT) has been advised as a remedy for postmenopausal women to combat some of the unfavourable elements of menopause, and there are some obvious benefits of HRT in terms of muscle performance control ( Chidi-Ogbolu N, Baar K, “Effect of Estrogen on Musculoskeletal Performance and Injury Risk”, 2019).
According to research from Wilfrid Laurier University’s Department of Kinesiology and Physical Education, hormone replacement therapy (HRT) combined with exercise has been proposed as potentially therapeutic agents for postmenopausal women, as these agents may potentially limit muscle damage and inflammation and stimulate repair in the musculoskeletal structures in regards to joint pains.
Aside from HRT, there are additional therapies and management techniques for menopausal joint pain. The following discussion will go into numerous techniques to efficiently manage and treat joint symptoms during menopause, ranging from lifestyle changes to alternative therapy. These developments will provide a more complete understanding of the available possibilities for increasing quality of life during this vital stage.
How to Treat Menopausal Joint Pains?
Menopausal joint pain can be efficiently treated with a mix of lifestyle changes, medication, and alternative therapies. Regular physical activity, according to studies, can dramatically reduce joint pain and stiffness. Low-impact workouts, such as swimming or cycling, help to maintain joint flexibility without putting too much load on the joints. Below are list of potential alternatives for treating menopausal joint pain:
Regular Exercise/Workouts
This can help preserve and strengthen the heart, bones, and muscles. It will aid in the maintenance and improvement of balance, body weight, and mood general well-being. Exercise should be varied to incorporate cardiovascular, strength training, and stretching. Walking, yoga, swimming, and mild Pilates have all been discovered to be beneficial. Avoid high-impact exercises such as sprinting and jumping as excessive tension is applied to joints.
Unwind
Pain threshold levels can be reduced when progesterone levels are low as well as decreased mood and peacefulness. It is important to schedule time for relaxing throughout the day. Because everyone is unique, try a variety of ways to find one that works for you. Relaxation techniques include cognitive behavioural therapy (CBT), mindfulness, breathing exercises, visualisation exercises, reading, and listening to soothing music.
Lose Weight
The body’s capacity to convert fat into muscle is affected by low testosterone levels, and the amount of fat around your abdomen is increased by low oestrogen levels. The normal BMI range is between 18.5 and 24.9. Higher BMI levels might put more strain on joints.
Supplementation
A dietary supplement known as soy isoflavone has been studied for the treatment of menopausal symptoms. It can be found in soy, legumes, and kudzu. In both animal and randomised controlled trials, these supplements showed improved bone mineral density and cartilage degeneration significantly. Other supplements, such as phytoestrogens, evening primrose oil, starflower oil, fish oils, or ginseng, have been reported to be utilised for postmenopausal non-vasomotor symptoms, including arthralgia.
Medication and Therapies
Hormone replacement treatment (HRT) has been utilised to minimise muscle and bone loss and restore muscle protein balance to offset many of the unfavourable characteristics of menopausal joint aches. Drugs that target inflammatory mediators for pain control have traditionally been employed, but they may miss the underlying cause of arthralgia and have nothing to do with oestrogen receptor impact on the joint itself during menopause.
While these methods may provide temporary relief, it is of the utmost importance to identify the possible link between menopause and the development or exacerbation of other joint-related illnesses, such as osteoarthritis. If joint pain persists or increases, consult us at OMC to rule out other joint illnesses and explore other treatment options, highlighting the importance of seeking medical help in such cases.
Is there a Connection Between Menopausal Arthralgia and other Joint Conditions?
Yes, there is a link between menopausal arthralgia and the worsening of various joint diseases. The reduction in oestrogen levels during menopause has been linked to an increased risk of developing or worsening joint disorders such as osteoarthritis (OA) and stiffness.
According to study in the Journal of Maturitas, osteoarthritis (OA) affects 18% of women over 60 and is the most prevalent joint ailment worldwide. They are frequently linked with increased pain, joint stiffness and painful leg aches. Radiological abnormalities linked with an OA diagnosis include articular cartilage breakdown with accompanying joint space loss, osteophyte formation, subchondral bone sclerosis, and cyst formation.
It’s crucial to know that the length of menopausal joint aches can vary as we examine their persistence. Some women may feel relief after menopause, while others may observe similar symptoms lingering, indicating the likelihood of chronic illnesses such as osteoarthritis.
In the next section we will go into detail on the average length of joint pains with relation to menopause.

How Long Does Menopausal Joint Pain Usually Last?
The duration of menopausal joint pains varies greatly amongst women, typically lasting several years. Menopausal symptoms can appear months or years before your periods stop and might linger for years afterwards. If you experience menopause as a result of surgical or medical procedures, you will most likely experience the symptoms of menopause much more gradually.
The frequency of menopausal joint pain (arthralgia) appears to rise in women going through menopause, which is thought to be due to a drop in oestrogen levels and this highlights the issue of proactive prevention. Due to the rise of cases of women suffering from joint pains, there is growing interest in determining preventive measures, such as regular physical activity, maintaining a healthy weight, and consuming joint-supporting nutrients. These can reduce the risk or severity of joint discomfort before it develops.
It is essential to identify symptoms as soon as they do so and to consult a healthcare professional. This proactive healthcare consultation plays an important role in navigating various medications or interventions, leading us to investigate whether menopausal joint troubles should be addressed by a doctor.
When Should You See a Doctor?
Menopausal joint pains should be discussed with a doctor if they continue or severely interfere with everyday life because they may not necessarily be caused by the menopause, but rather may be a sign of more serious, underlying health problems.
Persistent, severe, or worsening joint pain, especially if accompanied by swelling, redness, or restricted motion, should be checked medically to rule out disorders such as arthritis, osteoporosis, or autoimmune diseases, which can emerge around menopause.
At OMC, we’re here to assist you discuss these challenges and provide guidance targeted to your specific circumstances. You’ll avoid long lines and gain fast access to a plethora of menopausal knowledge when you work with us.
Contact us today to see how we may assist you with your symptoms.